-
Doctors believe that it is generally good for people who have had a coronavirus infection to be vaccinated if they do not have symptoms or an active infection.
-
An advisory committee to CDC suggested that individuals should wait 90 days after their infection, as reinfection is unlikely during the period.
-
However, for patients with chronic coronavirus symptoms, it is unclear whether the vaccine may exacerbate an existing inflammatory response.
-
For this reason, doctors say it is best to keep these individuals out.
-
Visit Business Insider’s homepage for more stories.
Individuals who have previously had COVID-19 are at the bottom of the U.S. vaccination priority list.
Emerging research suggests that immunity to the virus can last from a few months to a few years, so U.S. officials remain focused on getting shots for those who may become ill for the first time.
“We want to look at vaccinating patients who are not infected with COVID and who are susceptible,” Todd Ellerin, director of infectious diseases at South Shore Health in Massachusetts, told Business Insider earlier. “The patients after COVID are not your first, second, third or fourth group of groups you are going to want to vaccinate.”
However, it is not forbidden to get the shots of people who were previously infected if they are in a priority group such as health care workers or residents of nursing homes.
Both Pfizer and Moderna’s late-stage clinical trials suggest that the vaccines are safe for individuals with a history of coronavirus infections – and are likely to be just as effective in this group as among healthy individuals.
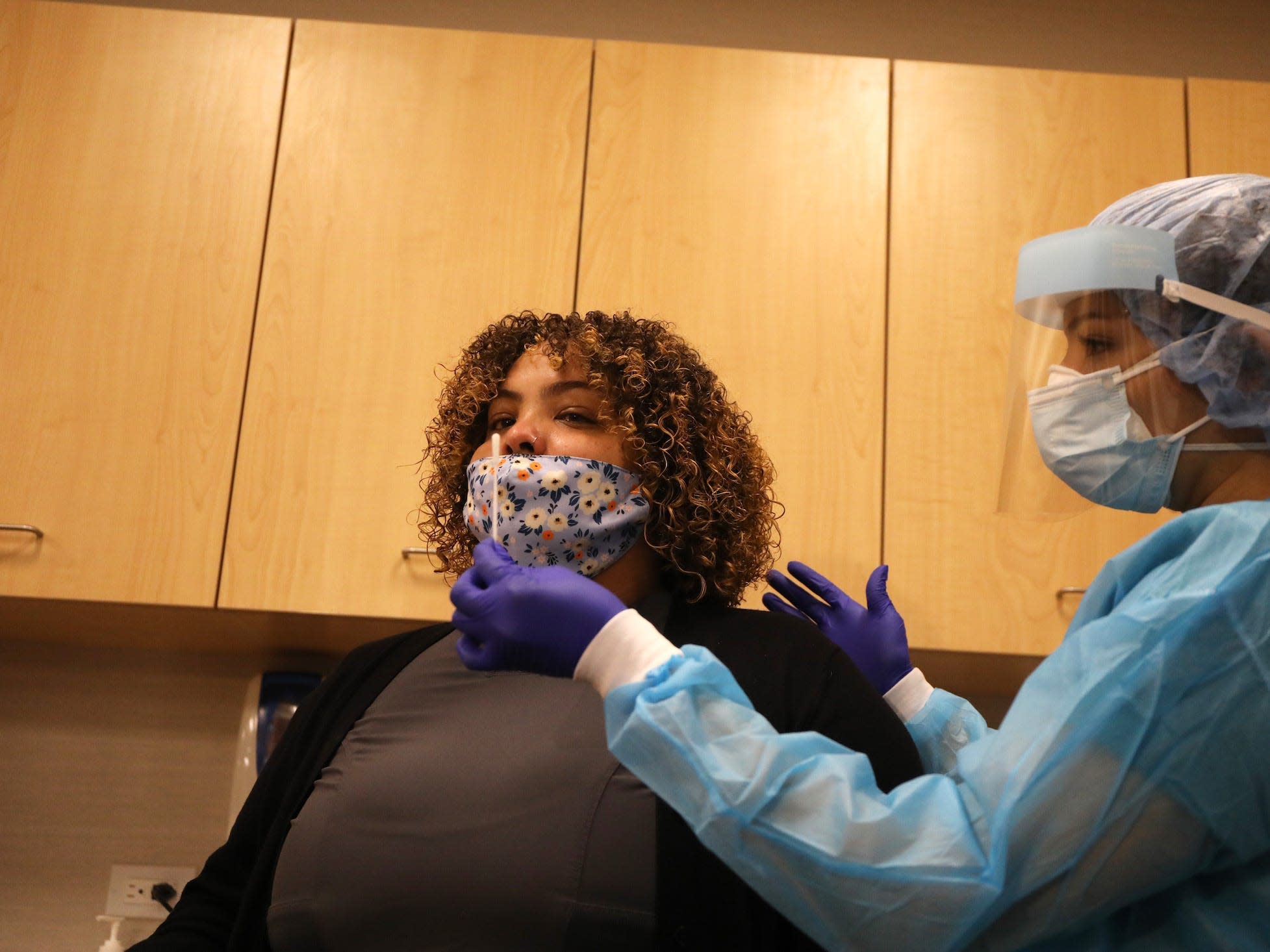
However, there are some exceptions. The Centers for Disease Control and Prevention recommends that people with an active infection wait until their symptoms have disappeared – and the standard ten-day isolation period is over – before being vaccinated. This includes people who have already received the first dose in the two-dose treatment of the vaccine.
“The recommendations for receiving any dose of the vaccine are not to get if you are currently seriously ill,” said Dr Sandra Sulsky, an epidemiologist and principal at Ramboll, a global health sciences consulting firm. Business Insider said.
In December, a CDC advisory committee said individuals with access to a vaccine could wait 90 days after their initial infection on the first shot if they wished, as re-infection during this period is unlikely.
“In terms of whether the vaccine is needed to prevent reinfection, I generally believe that it can not hurt, and it can help,” said Dr. Steven Deeks, a professor of medicine at the University of California, San Francisco. , Business Insider said. “So for the general population who did well after COVID, [if] it’s three months, get a vaccine. ‘
But for people who continue to experience long-term symptoms, the CDC has not yet made a recommendation. This is because researchers are not yet sure what causes these persistent ailments.
Doctors are currently suggesting that these patients should no longer be vaccinated.
What clinical trials have told us so far

Pfizer did not screen participants for evidence of a previous coronavirus infection during its late-stage clinical trial. It therefore appears that 3% of the participants were previously infected. According to the data, the vaccine is just as effective in this group, but according to the Food and Drug Administration, there is not enough evidence to know whether the vaccine re-infection occurs.
In the trial of Moderna, 2.2% of the participants had been infected before.
“It was a small number, so their stats aren’t particularly robust, and you can’t really rely on that much,” Sulsky said.
If a person is no longer symptomatic, doctors say there is a small risk of an adverse reaction, based on the history of coronavirus infection alone.
Read more: What comes next for COVID-19 vaccines? Here’s the latest on 11 leading programs.
Instead, it is the “long throwers” – patients with the coronavirus whose symptoms last three weeks or longer – who are still cheating doctors.
‘It will be difficult to start a long-term business [a vaccine] study whether they have ongoing health problems, “Natalie Lambert, an associate professor of medicine at Indiana University, previously told Business Insider.” Ethically, there would be big problems getting them vaccinated. “
Deeks said it is likely that some long-term importers will be vaccinated anyway, either in clinical trials or as part of general vaccinations in the US. Eventually, therefore, scientists can obtain enough data to know whether the shots are safe for this group.
Long distance guards have to wait

The FDA said there was “insufficient data” to determine whether coronavirus vaccines are safe for people with a weakened immune system. It is possible that long guards may fall into this category.
This makes it difficult for doctors to give individual advice on whether long-distance patients should be vaccinated.
“It would certainly make sense to consult with your primary care provider, but since no one knows what to do, you are not really going to get advice from a knowledgeable expert,” Deek said.
Currently, there are two prevailing theories as to why some people develop long-term symptoms.
The most plausible explanation, Deeks said, is that long-term coronavirus symptoms are related to an inflammatory response initiated by the virus. In that case, he added, the vaccine could make the inflammatory response even worse.
“It’s easier to argue that it would do more harm than good,” Deeks said. “If there is no information and it is not urgently needed to get a vaccine, I will wait.”
The other idea, he said, is a theoretical argument that there is a persistent infection that is causing the symptoms and that if you improve your immune response to the infection through a vaccine, you will get rid of the infection and you will get better. “
But the theory, he added, “seems very unlikely.”
Read the original article on Business Insider