By Nancy Lapid
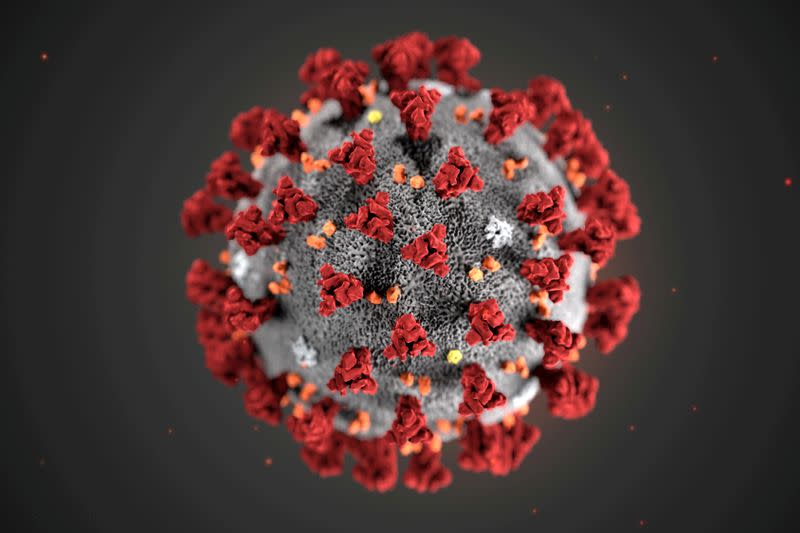
(Reuters) – The following is a summary of some of the latest scientific studies on the new coronavirus and efforts to find treatments and vaccines for COVID-19, the disease caused by the virus.
Some cold antibodies can help fight COVID-19
Antibodies to the six coronaviruses that cause colds cannot “neutralize” the coronavirus that causes COVID-19, but antibodies to two of them can at least help the body ward off serious diseases from the new virus, a small pre-study on. German researchers studied 60 patients with COVID-19, including 25 who were admitted to hospital but were not critically ill, 19 who needed admission to the intensive care unit, and 25 who did not become ill enough to be hospitalized. to be admitted. The patients requiring intensive care all have significantly lower levels of antibodies against two seasonal coronaviruses, HCoV OC43 and HCoV HKU1, which the authors say are more closely related to the COVID-19 virus compared to the other human coronaviruses. Although the observation does not prove that these antibodies are responsible, “it is noteworthy that the effect of HCoV OC43 and HKU1-specific antibody levels in such a small study reached a statistical significance with respect to the need for intensive care therapy, the “Further studies need to validate this finding and investigate the potential for identifying individuals at risk for serious disease outbreaks before a SARS-CoV-2 infection,” the researchers said in a statement published Tuesday in the International Journal of Infectious Diseases. (https://bit.ly/3aMvaqd)
The side effects of vaccines can affect mammograms
Routine mammograms should be done before the first dose of a COVID-19 vaccine or four to six weeks after the second dose, the Breast Imaging Association recommends. The temporary side effects of the vaccines may include swollen lymph nodes around the armpits, which can be misread as a possible sign of breast cancer if it appears on a mammogram. So-called armpit-shaped lymphadenopathy is usually only seen according to 0.02% -0.04% of mammographic examinations according to the Association’s guidelines. In trials with the Moderna vaccine, the condition develops in 11.6% of participants after the first dose and in 16% after the second dose. Researchers who tested the Pfizer / BioNTech vaccine did not frequently ask participants about the softness of the armpit and swelling of lymph nodes, but some people reported this side effect, which lasted an average of 10 days. Subtle effects on lymph nodes visible only on X-rays are likely to last longer, the Association said, although it is not yet clear what the vaccination-related lymph node changes look like there. “As more information is available on the occurrence and incidence of axillary lymphadenopathy after COVID-19 vaccination, it may be appropriate to change the duration of the follow-up or final assessment recommendations,” the Association said. (https://bit.ly/2MmkQvR)
Nursing staff delayed in COVID-19 vaccinations
Nursing home residents are among the most vulnerable to severe COVID-19, but vaccinations appear to be lagging behind among staff members caring for them. By mid-January, approximately 714,000 U.S. nursing home residents and 582,000 staff members had received at least one dose of COVID-19 vaccine, researchers from the U.S. Centers for Disease Control and Prevention (CDC) estimated. When nursing homes were grouped by state, the average percentage of vaccinated residents ranged from 68% to 100%, while the average percentage of vaccinated staff ranged from just 19% to 67%, the CDC said. In a commentary published in JAMA on Wednesday, CDC researchers said that on average nationwide, no more than about a third of staff in the nursing home have been vaccinated. This is of concern because this population has an occupational risk for exposure to SARS-CoV-2. . “They said barriers to vaccination of staff, including shift work schedules and the lack of paid sick leave due to vaccination side effects, need to be addressed.” Communication and outreach strategies are needed to improve vaccination among this priority population, “they said. said. (https://bit.ly/3soiwns; https://bit.ly/3bBmUsj)
Celiac disease does not increase COVID-19 risks
New data show that celiac disease does not increase the risk of infection or serious illness due to the new coronavirus. People with celiac disease lack immune activity and are known to be more vulnerable to a variety of viral infections, raising concerns that they may also be more vulnerable to COVID-19. But when researchers in Sweden used national databases to compare 40,963 people with celiac disease with 183,892 similar people without them, they found no differences in the risks of infection, COVID-19 hospitalization, critical illness requiring intensive care or death due to the disease does not. In a report published in Clinical Epidemiology on Thursday, the authors note that Sweden has introduced only limited social distance prescriptions, and ‘the lack of general lock-in is likely to have increased the number of individuals exposed to COVID-19.’ In this environment, they report, the risk of hospitalization for COVID-19 was approximately 1-in-1000 and the risk of being diagnosed with COVID-19 was approximately 1%. “There was no difference in these outcomes when comparing patients with celiac disease with controls.” (https://bit.ly/3qRw9uY)
Open https://tmsnrt.rs/3c7R3Bl in an external browser for a Reuters image on vaccines being developed.
(Reporting by Nancy Lapid; Edited by Bill Berkrot)