UC San Francisco scientists have discovered a new way to control the immune system’s “natural killer” (NK) cells, a finding with implications for new cell therapies and tissue implants that can evade immune rejection. The findings could also be used to question the ability of cancer immunotherapies to detect and destroy veil tumors.
The study, published today (January 8, 2021) in the Journal of Experimental Medicine, addressed a major challenge for the field of regenerative medicine, said lead author Tobias Deuse, managing director, Julien IE Hoffman, managing chair in cardiac surgery in the UCSF Division of Surgery.
“As a heart surgeon, I would like to put myself out of action by being able to implant healthy heart cells to repair heart disease,” Deuse said. He is interim chairman and director of minimally invasive cardiac surgery in the Division of Cardiothoracic Surgery for Adults. . ‘And there is great hope that one day the insulin-producing cells will fit in patients with diabetes or to inject cancer patients with immune cells designed to search for and destroy tumors. The biggest obstacle is how to do it in a way that avoids immediate rejection by the immune system. ‘
Deuse and Sonja Schrepfer, MD, PhD, also a professor in the Department of Surgery’s transplant and stem cell immunobiology laboratory, study the immunobiology of stem cells. They are world leaders in a growing scientific subfield working to produce “hypo-immune” cells and tissues in laboratories – which can avoid detection and rejection by the immune system. One of the most important methods to do this is to design cells with molecular guard codes that activate immune cell “switches”, called immune checkpoints, which normally help prevent the immune system from attacking the body’s own cells and modulating the intensity of immune responses to to avoid excess. collateral damage.
Schrepfer and Deuse recently used gene modification tools to design hypo-immune stem cells in the laboratory that are effectively invisible to the immune system. These cells can not only avoid the learned or “adaptable” immune responses of the body, but also the automatic “innate” immune response of the body against possible pathogens. To achieve this, the researchers adapted a strategy used by cancer cells to keep innate immune cells at bay: they designed their cells to release significant levels of a protein called CD47, which shuts down certain innate immune cells. by activating a molecular switch on it. cells, called SIRPα. Their success has become part of the founding technology of Sana Biotechnology, Inc., a co-founder of Schrepfer, who is now leading a team developing a platform based on these hypo-immune cells for clinical use.
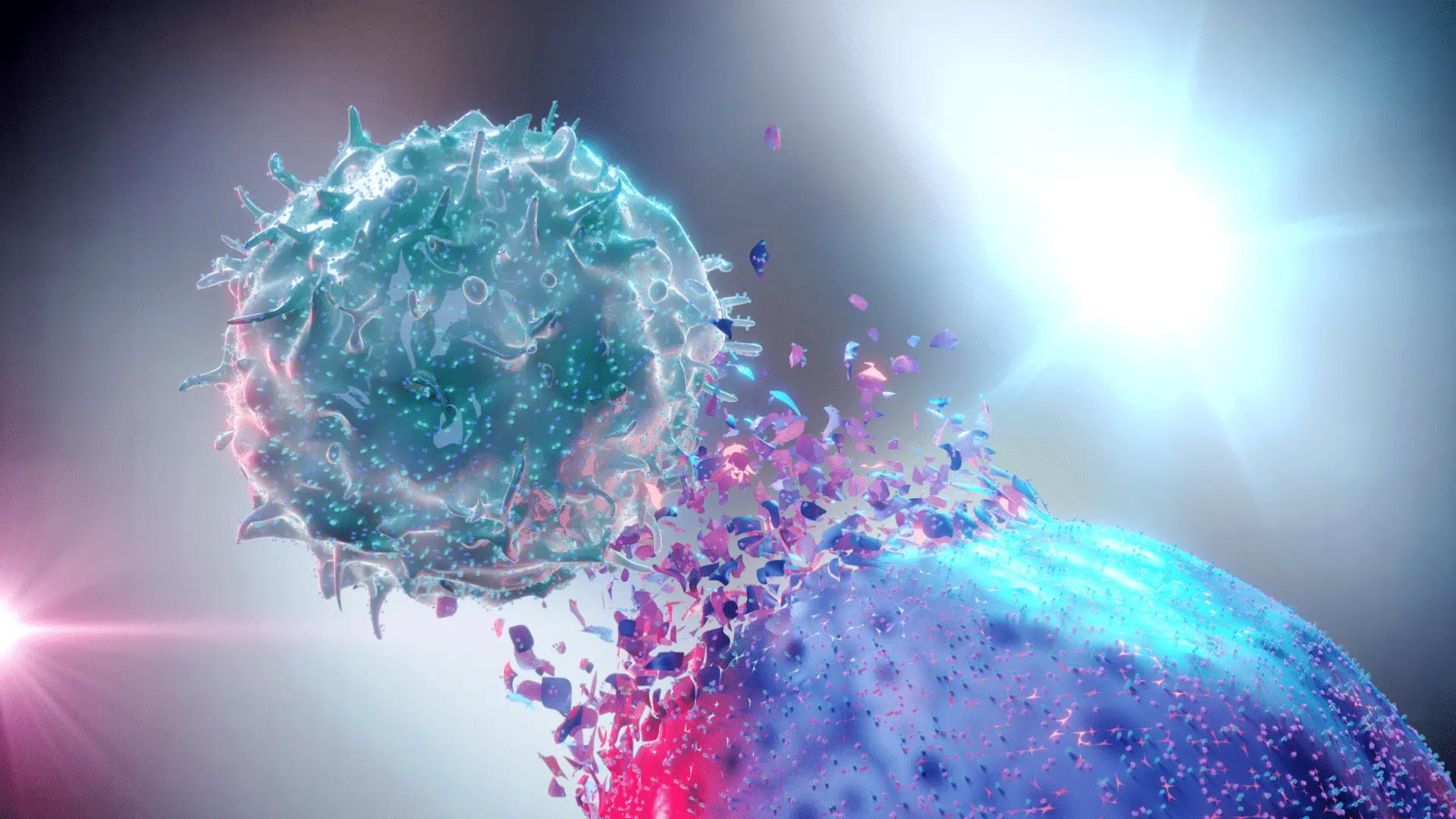
But the researchers left a mystery on their hands – the technique was more successful than predicted. In particular, the field was surprised that such engineered hypo-immune cells could deftly evade detection by NK cells, a type of innate immune cell that is not supposed to express a SIRPα control point at all.
NK cells are a type of white blood cell that responds as an immunological first reaction and can quickly detect and destroy any cells without the correct molecular ID proving that it is ‘self’ – indigenous body cells or at least permanent residents – that takes shape. of highly individualized molecules called MHC class I (MHC-I). When MHC-I is artificially knocked out to prevent transplant rejection, the cells become susceptible to accelerated NK cell killing, an immunological rejection that no one in the field has yet been able to fully inhibit. The data from Deuse and Schrepfer from 2019, published in Nature Biotechnology, suggested that they may have come across a switch that could be used for that purpose.
“All the literature said that NK cells did not have this checkpoint, but when we looked at cells from human patients in the laboratory, we found SIRPα there, like the day before,” Schrepfer recalls. “We can clearly show that stem cells that we design to overexpress CD47 can turn off NK cells in this way.”
To examine their data, Deuse and Schrepfer approached Lewis Lanier, PhD, a world expert in NK cell biology. Initially, Lanier was sure there must have been an error because several groups had already searched for SIRPα in NK cells and it was not there. But Schrepfer was confident in the data of her team.
“It finally hit me,” Schrepfer said. ‘Most studies looking for checkpoints in NK cells were done in perpetually laboratory cultured cell lines, but we studied primary cells directly from human patients. I knew it had to be the difference. ”
Further investigation revealed that NK cells only begin to express SIRPα after being activated by certain immune signaling molecules, called cytokines. As a result, the researchers realized, this inducible immune point only acts in already inflammatory environments and can probably modulate the intensity of NK cells’ attack on cells without proper MHC class I identification.
“NK cells have been a major obstacle to the growing interest in the field in the development of universal cell therapy products that can be transplanted” off the shelf “without rejection, so these results are very promising,” said Lanier, chairman and J. Michael Bishop, a leading professor, said. in the Department of Microbiology and Immunology.
In collaboration with Lanier, Deuse and Schrepfer extensively documented how CD47-expressing cells can silence NK cells via SIRPα. While other approaches can silence some NK cells, this was the first time anyone could completely inhibit them. In particular, the team found that the sensitivity of NK cells to CD47 inhibition is very species-specific, consistent with its function of distinguishing ‘self’ from potentially dangerous ‘others’.
As proof of this principle, the team designed adult human stem cells with the rhesus macaque version of CD47, then implanted them in rhesus monkeys, where they successfully activated SIRPα in the NK cells of the monkeys and avoided the transplanted human to kill cells. In the future, the same procedure could be performed in reverse, expressing human CD47 in pig heart cells, to prevent them from activating NK cells when transplanted into human patients.
‘Currently, CAR T-cell therapies for cancer and new forms of regenerative medicine depend on being able to extract cells from the patient, change them in the laboratory and put them back in the patient. “It avoids the rejection of foreign cells, but is very difficult and expensive,” said Schrepfer. “Our goal to set up a hypo-immune cell platform is to create off-the-shelf products that can be used to treat diseases in all patients everywhere.”
The findings may also have implications for cancer immunotherapy, as a way to promote existing therapies that seek to overcome the immune checkpoints that cancers use to avoid immune detection. “Many tumors have low levels of self-identifying MHC-I proteins and some compensate by overexpressing CD47 to keep immune cells at bay,” Lanier said. He is director of the Parker Institute for Cancer Immunotherapy at the UCSF Helen Diller Family Comprehensive Cancer Center. “This may be the sweet spot for antibody therapies targeted at CD47.”
Reference: January 8, 2021, Journal of Experimental Medicine.
Authors: the main authors of the study were Deuse and UCSF TSI laboratory research scientist Xiaomeng Hu; Lanier and Schrepfer were the senior authors of the study, and Schrepfer is a corresponding author. Other authors were Sean Agbor-Enoh of the Johns Hopkins School of Medicine and National Heart, Lung, and Blood Institute (NHLBI); Moon K. Jang at the NHLBI; Hannah Valantine at Stanford; Malik Alawi and Ceren Saygi of the University Medical Center Hamburg-Eppendorf in Germany; Alessia Gravina, Grigol Tediashvili and Vinh Q. Nguyen of UCSF; and Yuan Liu of Georgia State University.
Funding: The research and researchers are supported by NHLBI (R01HL140236), the Parker Institute for Cancer Immunotherapy and the U.S. National Institutes of Health (NIH P30 DK063720 NIH S10 1S10OD021822-01).
Disclosures: Deuse is co-founder and Schrepfer is scientific founder and senior vice president of Sana Biotechnology Inc. Xiaomeng Hu is now a senior scientist at Sana Biotechnology Inc. No reagent or any funding from Sana Biotechnology Inc. was not used in this study. UCSF has filed patent applications covering these inventions.