It is quite crowded in the bone marrow. Many types of stem and stem progenitors, including ancestors of immune cells, coexist1,2 and is supported by nearby cells that generate specialized protective environments for the stem cells called niches. The interaction between the cells of the niche, also known as stromal cells, and early progenitors of immune cells in the bone marrow is poorly understood. Insight into how these interactions are coordinated will help us better understand how progenitors are generated from immune cells. Subscribe Nature, Shen et al.3 solved part of the puzzle by identifying a role for movement to stimulate communication between one type of stromal cell and immune fathers in mice, which ultimately helps the animals fight infection.
The different types of stem and progenitor cell in the bone marrow are very interconnected, both physically and functionally. For example, mesenchymal stem and stem cells, which give rise to bone, skeletal tissue, and fat cells, are an essential part of the stromal niche for hematopoietic stem and stem cells (HSPCs). HSPCs in turn are responsible for the production of all bloodlines, including immune cells4. In mice, some mesenchymal progenitors produce a signaling protein called SCF, which is crucial for supporting HSPCs.5. These cells also express a cell surface protein called the leptin receptor5 (LepR). LepR expression (LepR+) cells are located in different places in bone marrow, including about two types of blood vessels, arterioles and sinusoids. The LepR+ population is a mixture of mesenchymal progenitor cells5. Shen et al. depart home for the LepR subset+ cells involved in the maintenance of the HSPC niche.
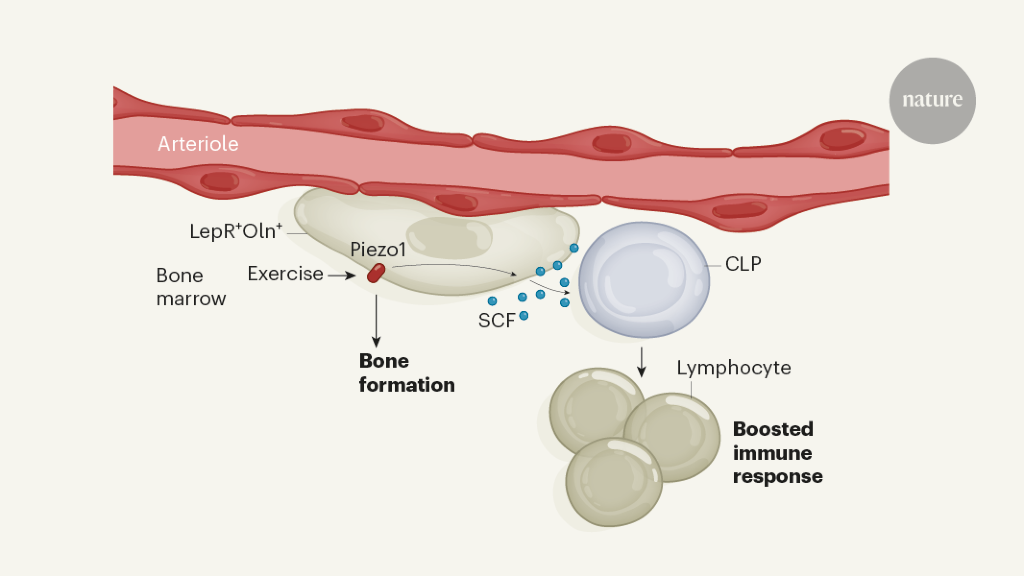
The authors performed a no-expression analysis of LepR+ cells, which revealed that one subpopulation also expresses another marker protein, osteolectin (Oln). The group generated mice in which this Oln+ cells fluorinated, and found that Oln+ stromal cells are around arterioles but not sinusoids. They then showed that the cells are short-lived osteogenic ancestors, giving rise to bone-forming cells called osteoblasts, which play a crucial role in bone regeneration.
Shen and colleagues designed mutant mice to shorten the gene containing SCF in Oln+ selle. The resulting lack of SCF in Oln+ cells have no effect on hematopoietic stem cells or most other types of hematopoietic progenitor cells in the bone marrow. However, this has led to a significant decrease in the number one special type of hematopoietic progenitor – the common lymphoid progenitor (CLP), which gives rise to immune cells called lymphocytes. In support of the idea that the Oln+ cells help generate and maintain CLPs, the authors showed that Oln+ cells and CLPs are close together in the bone marrow. They then infected the mutant mice with a disease-causing bacterium, Listeria monocytogenes, which is usually removed from the body by lymphocytes. The mutant animals cleared the pathogen much less effectively than the controls. The animals simply did not produce enough lymphocytes to do the job, due to the reduced number of CLPs.
It is known that mechanical stimulation of bones, which occurs during exercise, promotes bone formation6. In a final set of experiments, Shen et al. placed mice in cages with running wheels, and found that running resulted in a higher number of both Oln+ cells and CLPs in bone marrow. The group found that the Oln+ cells express the mechanosensitive ion channel protein Piezo1, and showed that the CLP numbers are abnormally low in mice designed to shorten this protein. The authors thus discovered a previously unknown pathway by which exercise, observed by the mechanosensitive protein Piezo1, causes SCF expression in osteogenic progenitors to maintain CLPs and thus control part of the function of the immune system (Fig. 1).
The discovery that megosensitive osteogenic progenitors play a role in combating bacterial infections is exciting. It was known that exercise can stimulate the immune system7, but the progress in the work of Shen and colleagues provides one reason why this is the case. If relevant to humans, the work may have direct clinical applications. The pathway exposed in the present study, for example, can be used to develop better therapies to strengthen the immune cell outputs caused by movement. A logical next step is to test whether voluntary running can improve bacterial clearance in mice. Another important question to address is whether increasing the number of Oln+ cells and CLPs in bone marrow would help provide protection against other disease-causing bacteria, or even viruses, or whether it could also promote vaccination.
The authors also found that the number of Oln+ niches, and the number of CLPs, were lower in the bone marrow of 18-month-old mice than in their 2-month-old counterparts. Elderly animals are also active8, so factors other than reduced movement may contribute to this aging-related decline.
It will be interesting to investigate, for example, whether the way Oln+ niches feel mechanical stimulation changes over time, or epigenetic changes (alterations to DNA that can alter gene expression without altering the underlying DNA sequence) in elderly Oln+ cells make them less effective in generating signaling molecules such as SCF.
Mechanosensing is well established to play a role in bone physiology, but an important role for mechanosignaling has also been described for other cell types – for example, pancreatic progenitor cells, intestinal stem cells, and the endothelial cells that carry blood vessels. Although less is known about the niches that support stem cells outside the bone marrow, the vascular system, and thus endothelial cells, are the best candidates for the formation of such niches. It is therefore possible that mechanosensing in niche-forming endothelial cells may contribute to the maintenance of other forms of stem and stem progenitors. If this is the case, the work of Shen and colleagues could have major consequences for stem cell biology.