By Nancy Lapid
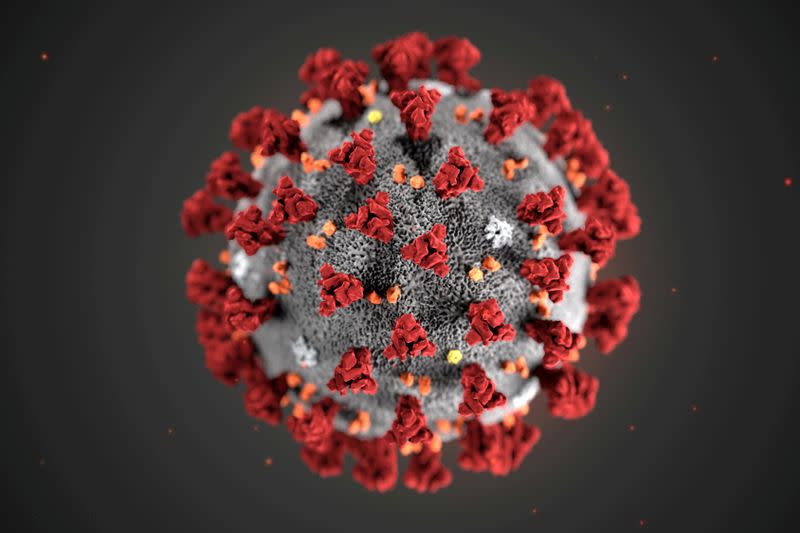
(Reuters) – The following is a summary of the latest scientific studies on the new coronavirus and efforts to find treatments and vaccines for COVID-19, the disease caused by the virus.
Blood type is not a factor in COVID-19 risks in US patients
Blood type does not affect COVID-19 susceptibility in American patients, a new study indicates. Researchers analyzed data on nearly 108,000 people from Utah, Idaho and Nevada who were tested on COVID-19 and whose blood type was listed in their medical records. None of the blood groups – A, B, AB or O – were linked to their risk of becoming infected, the need for hospitalization or intensive care, according to a report published in JAMA Network Open. Smaller studies from China, Italy, and Spain linked type A blood to higher COVID-19 risks and type O blood to lower risks, and a large study from Denmark linked blood type to COVID-19 severity. Studies from New York and Boston – such as this new study – found no such links. Study co-author Dr. Jeffrey Anderson of the Intermountain Healthcare Heart Institute in Salt Lake City said in a statement that the effects of blood type in the population can vary. “We’ve looked at a lot of risk factors about who might need to be hospitalized and who needs more advanced care, and … at least, for our population, blood type is not on the list,” Anderson said. (https://bit.ly/32rVzVb)
Asthma medication can prevent COVID-19 from getting lighter
An inhaled steroid commonly used to treat asthma can help make patients with mild COVID-19 sicker, according to the results of a trial published in The Lancet Respiratory Medicine. Within a week of developing symptoms, 73 patients were randomly assigned to receive inhaled budesonide twice daily, and another 73 were assigned to receive normal care only. Patients used budesonide for an average of 7 days. Finally, 15% of patients receiving regular treatment need an urgent visit or hospitalization, compared to only 3% of those treated with budesonide. Patients receiving budesonide also had fewer days with fever, fewer days to take medication to prevent fever, and recovered faster on average one day. “To our knowledge,” the researchers said, this is the first trial of corticosteroids inhaled in early COVID-19 disease, and it may provide the first easily accessible effective intervention for patients with mild symptoms. They said larger trials are urgently needed to confirm their findings, especially in setting up an early treatment that is widely available and relatively safe. (https://bit.ly/3e6p2K1)
Household members face a higher risk of infection from the British variant
Compared to people infected with less contagious coronavirus variants, those infected with the variant identified in the UK, known as B.1.1.7, according to new data are likely to be infected in their households. During three weeks in February, researchers in Ontario, Canada, monitored people living with a COVID-19 patient in more than 2,500 private households that were approximately comparable. During the two weeks after patients were diagnosed, the so-called secondary attack rate – the rate at which infections occurred among domestic members – was 31% higher when the patient was infected with the B.1.1.7 virus variant than when COVID-19 was caused by a less worrying variant. When the original infected person never developed symptoms, the secondary attack rate was 91% higher with B.1.1.7, the researchers reported on medRxiv before peer review. And when the original patient first had no symptoms and then became ill, the rate at which domestic members became infected was more than 200% higher when the patient wore the B.1.1.7 variant. Since its inception in the United Kingdom, B.1.1.7 has spread to more than 100 other countries. It has now become the dominant coronavirus variant in the United States, according to the U.S. Centers for Disease Control & Prevention. (https://bit.ly/32lfTHT)
Experimental portable monitors for COVID-19 cytokine storm
A portable “sweat sensor” could one day help monitor patients with COVID-19 and other diseases before triggering a cytokine storm, a surge of inflammatory proteins that announces a potentially fatal overreaction of the immune system. Cytokines are usually measured in blood. They can also be measured in sweat, but only in “passive” sweat – not the kind produced during exertion. “The big challenge is that we do not sweat much, especially not in air-conditioned environments,” Shalini Prasad of the University of Texas at Dallas said in a statement. In the wristwatch device her team is developing, small amounts of passive sweat spread on a sensor strip attached to an electronic reader. The reader detects any inflammatory proteins and sends the data wirelessly to a smartphone application. “Especially now in the context of COVID-19, if you could monitor pro-inflammatory cytokines and see that they are on the rise, you can treat patients early, even before they develop symptoms,” Prasad said. virtual meeting of the American Chemical Society. The researchers plan to initially test the device in patients with non-COVID respiratory infections, such as flu. (https://bit.ly/2RvJPij)
Open https://tmsnrt.rs/3c7R3Bl in an external browser for a Reuters image on vaccines in development.
(Reported by Nancy Lapid; edited by Bill Berkrot)